CAR-T cell therapy transforms relapsed Leukemia treatment with high remission rates
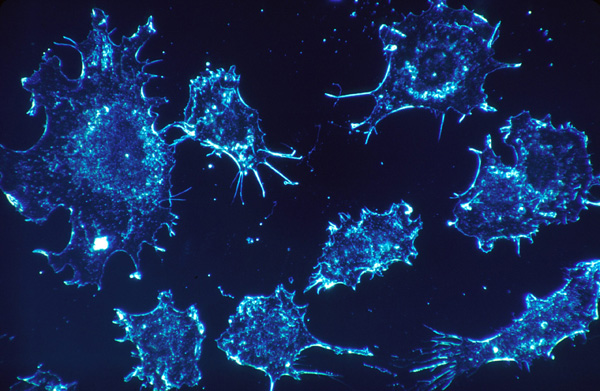
[An image of cancer cells. Photo Credit: Raw Pixel]
In a 2014 New England Journal of Medicine study, researchers led by Shannon L. Maude reported that CAR-T cell therapy achieved complete remission in about 70 to 90 percent of children and young adults with relapsed acute lymphoblastic leukemia.
In the past, patients with leukemia who relapsed had limited treatment options, but this new result reshaped how the disease is treated.
Chemotherapy often became ineffective and the last resort was usually hematopoietic stem cell transplantation.
This treatment can save lives, but it is also very risky and challenging, especially because it needs a matched donor and can cause serious side effects like graft-versus-host disease.
Recently, chimeric antigen receptor T (CAR-T) cell therapy has changed how doctors approach leukemia treatment.
CAR-T therapy utilizes the patient’s own T cells, a key component of the immune system. These T cells are taken out of the body and genetically changed so they can recognize leukemia cells.
After that, the modified cells are reinfused into the patient, where they directly target and eliminate cancer cells.
This treatment gained recognition because of its effectiveness.
This is particularly remarkable because many of these patients had not responded to any other treatments before.
For many years, hematopoietic stem cell transplantation has been considered the most potent treatment for high-risk leukemia.
It works by replacing damaged bone marrow with healthy stem cells, allowing new blood cells to grow.
However, this process is intense and dangerous.
Patients are required to undergo strong chemotherapy, and there is always a risk that the body will react badly to the transplanted cells.
Compared to this, CAR-T therapy uses the patient’s own cells, which reduces some of these risks.
In some cases, patients who respond well to CAR-T therapy may not even need a stem cell transplant afterward.
Even though CAR-T therapy holds immense promise, it still faces several limitations.
Some patients experience serious side effects like cytokine release syndrome (high fever) and nervous system problems (headaches, changes in consciousness) because the immune system becomes overly active.
Additionally, the treatment is very expensive (from $300,000 to $475,000) and not easy to make.
Other issues are a weakened immune system with an increased risk of serious infections, allergic reactions during the infusion, abnormal levels of minerals in the blood and an increased risk of second cancers.
Still, CAR-T therapy is important because it shows a new way to treat cancer.
Instead of relying solely on drugs or radiation, this therapy enables the immune system to fight cancer independently.
Hematopoietic stem cell transplantation remains crucial, but CAR-T therapy is slowly reshaping the future of leukemia treatment.
Science does not improve all at once.
CAR-T cell therapy is not perfect, but it has already helped many patients who previously had no hope.
With more research, this therapy could become even safer and more effective in the future.

- Noelle Chun / Grade 11 Session 12
- Marriotts Ridge High School

![THE HERALD STUDENT REPORTERS [US]](/assets/images/logo_student_us.png)
![THE HERALD STUDENT REPORTERS [Canada]](/assets/images/logo_student_ca.png)
